Photo credit to Dr. Manuel González Reyes
As a recreational athlete since I was 14 years old, I've had a number of bumps and bruises. In the last few years, I've had several joint problems which were diagnosed as tendinitis (or tendinopathy as it is now called). This is an attempt learn about my problems.
As is the case in most of sports medicine, questions surrounding tendons are not investigated in large, well-funded clinical trials. Much of this article relies on studies with small sample sizes, not because I am intentionally cherry-picking data but because better data is not available to my knowledge.
A tendon is the structure that connects muscles to bones enabling the contractile tissue of the muscle to exert force on the skeleton. Approximately 70% of the dry weight of the tendon is type I collagen (there are 5 types but Type I is by far the most common). The remaining 20-30% is proteoglycans, glycosaminoglycans, and other collagens [1].
"Overuse tendinopathy was traditionally considered an inflammatory status of the tendon and its adnexae, related to frequent or excessive use. Since degenerative change and little inflammation have been demonstrated at histology, the term 'tendinosis' has increasingly replaced that of 'tendinitis'. However, the histological descriptive terms "tendinosis" (a degenerative pathological condition with a lack of inflammatory change) and "tendonitis" or "tendinitis" (implying an inflammatory process) should be used only after histopathological confirmation. At histology, peritendinitis and failed healing response, also defined 'tendinosis', have increasingly allowed to consider the overuse tendinopathy a "failed healing response" to overuse tendon injury, with haphazard proliferation of tenocytes, intracellular abnormalities in tenocytes, disruption of collagen fibers, and a subsequent increase in non-collagenous matrix." - [2]
Research into tendon pain is a young field. Diagnositic criteria are still being debated in the literature and single diagnoses are being applied to heterogeneous collections of symptoms without a mechanistic understanding of the underlying pathology. This makes reviewing the literature as a layperson difficult to impossible. For example, as of 2020, we are still using tiny sample sizes (n<20) to document symptom heterogeneity [3].
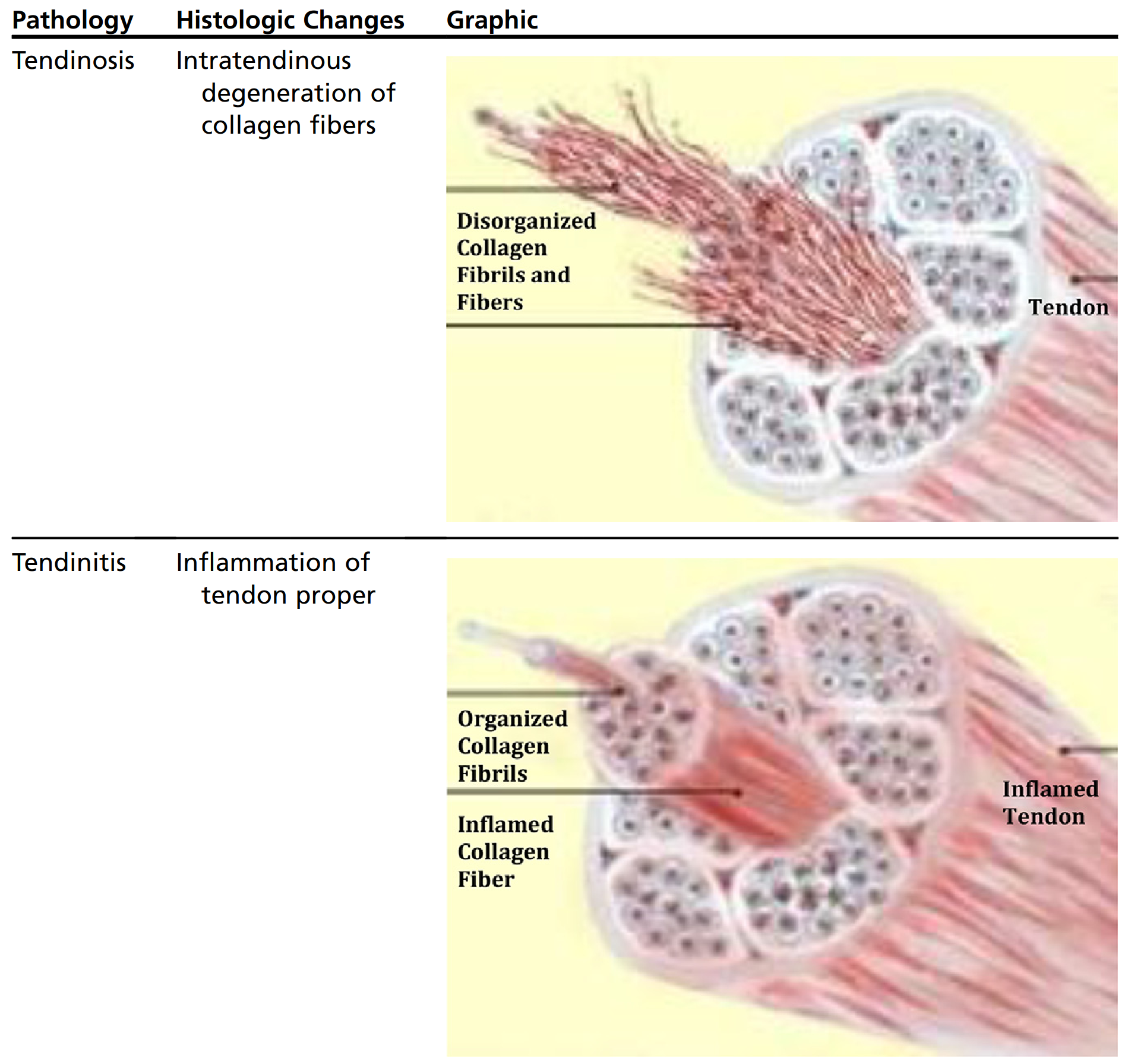
[Caption] Table from [4].
The etiology of tendon pain is long disputed but we do know that detectable changes in tendon structure are associated with tendon pain but that association is far from causal. For example, if tendon abnormalities visualible on an ultrasound in an asymptomatic patient, tendon pain is five times more likely in the future [5].
Tendinopathy affects lots of athletes as illustrated by the hodgepodge of studies on the prevalence: nine of 17 patients quit their sport as a result of patellar tendinopathy [6]; 20% of youth basketball players (male or female) are affected by patellar tendinopathy in a season [7]; 16 of 119 elite German soccer players had symptoms of patellar tendinopathy [8]; of 100 patients presenting to a sports medicine clinic with patellar tendinopathy, 33 were unable to return to play in 6 months and 18 were unable to return in 12 months [9].
Treatment options available can be roughly categorized as pharmaceutical, load and training (the physical therapy model), or surgerical intervention. At best, most of these interventions are controversial [10]. Surgical intervention is usually reserved for full tendon ruptures and is beyond the scope of this article.
The current literature is highly conflicted on loading based treatments. Most studies look at isometric, eccentric, or heavy slow resistance (usually a concentric/eccentric movement) loading for tendinopathy [11]. Unfortunately, these studies find conflicting and irreproducible results across populations.
For example in the case of patellar tendinopathy, isometric and heavy slow resistance training was effect in reducing symptions [12,13,14,15,16]. Eccentric training worsens tendinopathy [13]. Isometric training fails to provide pain relief in Achilles tendinopathy [17]. These examples are cherry-picked to show the contradictions in the literature but the point is that low quality studies are available to show almost anything.
Rather than focusing on the details of these contradictory studies, here is what the field currently seems to agree on. Rest is not good. It results in immediate pain relief but return to loading will increase pain because of tendon and muscle atrophy [18,19,20]. Loading, regardless of the form, should be titrated to the patient. The frequency, volume, and intensity of loading should be selected from a range near but not identical too the loading pattern that precipitated the injury [21,22,23,24,25]. Beyond these guidelines, certainty of outcome becomes impossible in the face of human variation in response to training. I believe this is responsible for the enormously conflicting body of literature on loading programs. Finding ways to continue loading these structures appears to be critically important but guidance on how much pain is harmful and under what conditions seems to be more of an artform among physical therapists rather than an exact science.
After sifting through dozens of reviews on the topic, this paper [26] said it best "No univocal evidence exists regarding the best non-operative management, which includes non-steroidal anti-inflammatory drugs, platelet-rich plasma (PRP), high volume image-guided injections, hyaluronic acid, and prolotherapy, for tendinopathy (in particular Achilles and patellar tendinopathies) as a suitable alternative to the commonly used eccentric loading rehabilitation regimen." Of these, NSAIDs and PRP are the most discussed in non-specialist (read "meathead") circles and in the scientific literature. The remaining options smell strongly of snake oil to me and nothing in my brief literature review challenged that assessment (for example, with hyaluronic acid - narrative rather than systematic reviews [27], hiding the number of study subjects deep in the paper [28]).
PRP is the process of extracting a patient's blood, separating out a platlet rich fraction by centrifugation, and reinjecting it into the patient at the site of injury in the hopes the healing factors in the plasma work more effectively in higher concentration. PRP is most evidence supported in recovery from surgery [29,30] but even there, evidence is not perfectly clear [31]. Literature reviews of PRP for tendinopathy consistently show more research is needed, that randomized controlled trials are using sample sized too small, and that while invitro studies are promising, the evidence is far from conclusively positive on PRP. It has not been shown to be more effective than saline injections in Achilles tendinopathy [32] and may or may not benefit patellar tendinopathy [33,34]. There is evidence that PRP warrants continued investigation but unless there are breakthroughs in the field yet to come, it is not going to be a panacea [35,36]. It seems to be a second or third line treatment option where positive results are hard to disentangle from the extra passage of time and physical therapy [37].
Because the role of inflammation in tendinopathy is highly debated, and tendinopathy itself is a heterogeneous collection of conditions (at least histologically), it is impossible to make blanket recommendations about the benefits of inflammation suppressing therapeutics [38]. However, NSAIDS, to the extent they can be recommended, are only recommended for acute tendinopathy [39,40].
What are your opinions on the role of tibilas raises for quadricep tendinopathy?
What are your opinions on the role of walking or sled dragging backwards for quadricep tendinopathy?
Is it worth investing in a leg extension machine for the management of quadricep tendinopathy?
What are your opinions on the role of nordic raises for general knee health?
Your recommendation for load titration in hip tendinopathy was very high pain levels. What are the differences (if any) in how you titrate load for quadricep tendinopathy (in the chronic presentation which is what I assume this is now)?
If I am not interested in dynamic loading of the tendon for now (years), does that change anything about the management approach?
Hip tendinopathy was expected to improve slowly over months; what is a reasonable expectation of recovery timeline for quadricep tendinopathy?
Is there a significant possibility that statins could be increasing my vulnerability to tendinopathy?
Are there any pertinent questions missing from this list? If yes, what are they and what are your answers?
[1] "Structure and function of ligaments and tendons," in Basic Orthopaedic Biomechanics and Mechano-biology, 2005.
[2] "Tendinopathy and inflammation: some truths," International Journal of Immunopathology and Pharmacology, vol. 24, pp. 45—50, 2011.
[3] "Self-reported jumpers' knee is common in elite basketball athletes—but is it all patellar tendinopathy?" Physical Therapy in Sport, vol. 43, pp. 58—64, 2020.
[4] "Tendonitis and tendinopathy: what are they and how do they evolve?" Foot and Ankle Clinics, vol. 22, pp. 665—676, 2017.
[5] "Can ultrasound imaging predict the development of Achilles and patellar tendinopathy? A systematic review and meta-analysis," British Journal of Sports Medicine, vol. 50, pp. 1516—1523, 2016.
[6] "Long-term prognosis for Jumper's knee in male athletes: prospective follow-up study," The American Journal of Sports Medicine, vol. 30, pp. 689—692, 2002.
[7] "The Burden and Risk Factors of Patellar and Achilles Tendinopathy in Youth Basketball: A Cohort Study," International Journal of Environmental Research and Public Health, vol. 18, pp. 9480, 2021.
[8] "Patellar tendinopathy in young elite soccer—clinical and sonographical analysis of a German elite soccer academy," BMC Musculoskeletal Disorders, vol. 18, pp. 1—7, 2017.
[9] "A cross sectional study of 100 athletes with jumper's knee managed conservatively and surgically," British Journal of Sports Medicine, vol. 31, pp. 332—336, 1997.
[10] "Controversies in tendinopathy treatments," Sportsfisio, 2017.
[11] "Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in individuals with patellar tendinopathy: A systematic review," Physiotherapy Research International, vol. 23, pp. e1721, 2018.
[12] "Fibril morphology and tendon mechanical properties in patellar tendinopathy: effects of heavy slow resistance training," The American Journal of Sports Medicine, vol. 38, pp. 749—756, 2010.
[13] "Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial," Journal of Science and Medicine in Sport, vol. 19, pp. 702—706, 2016.
[14] "Efficacy of an inertial resistance training paradigm in the treatment of patellar tendinopathy in athletes: a case-series study," Physical Therapy in Sport, vol. 12, pp. 43—48, 2011.
[15] "Isometric contractions are more analgesic than isotonic contractions for patellar tendon pain: an in-season randomized clinical trial," Clinical Journal of Sport Medicine, vol. 27, pp. 253—259, 2017.
[16] "Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy," British Journal of Sports Medicine, vol. 49, pp. 1277—1283, 2015.
[17] "Isometric exercises do not provide immediate pain relief in Achilles tendinopathy: A quasi-randomized clinical trial," Scandinavian Journal of Medicine & Science in Sports, vol. 30, pp. 1712—1721, 2020.
[18] "Current trends in tendinopathy management," Best Practice & Research Clinical Rheumatology, vol. 33, pp. 122—140, 2019.
[19] "Treatment options for patellar tendinopathy: critical review," Current Sports Medicine Reports, vol. 10, pp. 255—270, 2011.
[20] "Ten treatments to avoid in patients with lower limb tendon pain," British Journal of Sports Medicine, vol. 52, pp. 882—882, 2018.
[21] "Increased supraspinatus tendon thickness following fatigue loading in rotator cuff tendinopathy: potential implications for exercise therapy," BMJ Open Sport & Exercise Medicine, vol. 3, pp. e000279, 2017.
[22] "Gluteal tendinopathy: integrating pathomechanics and clinical features in its management," Journal of Orthopaedic & Sports Physical Therapy, vol. 45, pp. 910—922, 2015.
[23] "High-volume image-guided injections in Achilles and patellar tendinopathy in a young active military population: a double-blind randomized controlled trial," Orthopaedic Journal of Sports Medicine, vol. 10, pp. 23259671221088326, 2022.
[24] "Kinematic and kinetic differences between military patients with patellar tendinopathy and asymptomatic controls during single leg squats," Clinical Biomechanics, vol. 62, pp. 127—135, 2019.
[25] "Lecture: Isometric exercise in tendinopathy," Sportsfisio, 2017.
[26] "Current pharmacological approaches to the treatment of tendinopathy," Expert Opinion On Pharmacotherapy, vol. 21, pp. 1467—1477, 2020.
[27] "The role of hyaluronic acid in sport-related tendinopathies: A narrative review," Medicina, vol. 57, pp. 1088, 2021.
[28] "Efficacy and tolerability of peritendinous hyaluronic acid in patients with supraspinatus tendinopathy: a multicenter, randomized, controlled trial," Sports Medicine-Open, vol. 3, pp. 1—8, 2017.
[29] "Platelet-rich plasma: Growth factor enhancement for bone grafts," Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, vol. 85, pp. 638—646, 1998.
[30] "The use of platelet-rich plasma to enhance the success of bone grafts around dental implants," Dental Implantology Update, vol. 11, pp. 17—20, 2000.
[31] "Platelet-rich plasma: evidence to support its use," Journal of Oral and Maxillofacial Surgery, vol. 62, pp. 489—496, 2004.
[32] "Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial," JAMA, vol. 303, pp. 144—149, 2010.
[33] "Platelet-rich plasma in the treatment of patellar tendinopathy: a systematic review," The American Journal of Sports Medicine, vol. 43, pp. 2583—2590, 2015.
[34] "Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial," The American Journal of Sports Medicine, vol. 42, pp. 610—618, 2014.
[35] "The effectiveness of platelet-rich plasma in the treatment of tendinopathy: a meta-analysis of randomized controlled clinical trials," The American Journal of Sports Medicine, vol. 45, pp. 226—233, 2017.
[36] "Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review," PM&R, vol. 5, pp. 169—175, 2013.
[37] "Platelet-rich plasma: evidence for the treatment of patellar and Achilles tendinopathy—a systematic review," Musculoskeletal Surgery, vol. 99, pp. 1—9, 2015.
[38] "A systematic review of inflammatory cells and markers in human tendinopathy," BMC Musculoskeletal Disorders, vol. 21, pp. 1—13, 2020.
[39] "Rehabilitation of patellar tendinopathy," Journal of Musculoskeletal & Neuronal Interactions, vol. 20, pp. 535, 2020.
[40] "Patellar Tendinopathy:“Jumpers Knee”," Tendons, pp. 57—68, 2019.